

With extensive training, experience, and dedication to patient care offering the comprehensive services tailored to meet the unique needs of each individual.
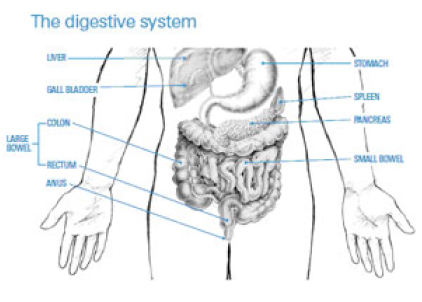
The Intestine is the part of the digestive system that is the longest—the “gut.” The long tube that begins at the back of the mouth and connects the stomach and intestines to the anus is the digestive system. It circulates within the body.
The “rectum”, which measures approximately 15 centimeters in length, and the “colon”, which measures approximately 1.5 meters in length. Through the anus, the rectum connects to the outside of the body.

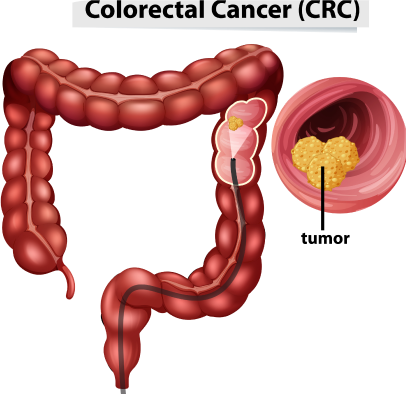
Colon cancer, also known as colorectal cancer, is a type of cancer that develops in the colon or rectum. It typically starts as small, noncancerous growths called polyps, which can gradually transform into cancer over time.
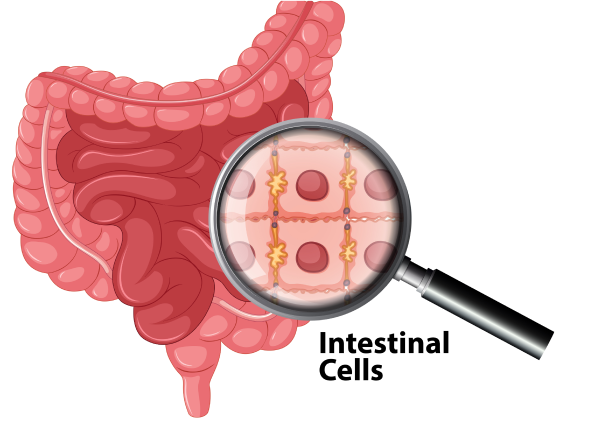
Polyps, small outgrowths of the inner lining of the intestine resembling mushrooms, can serve as the starting point for intestinal cancer. People over the age of 50 frequently develop these polyps, which are typically not cancerous. However, some polyps have the potential to develop into cancer.
It is unclear what exactly causes cancer of the intestines. The causes of colon cancer include a combination of genetic, lifestyle, and environmental factors, such as family history of colorectal cancer or polyps, age, certain genetic conditions etc.
Having ulcerative colitis, where the lining of the colon is inflamed, for more than eight to ten years.
Explore the diverse array of factors associated with colon cancer, ranging from genetic predisposition to lifestyle choices and dietary habits.
You should see a doctor for a checkup if you have any of the symptoms for longer than two weeks. To check for early signs of intestinal cancer, a faecal occult blood test (FOBT) can be performed. This test looks for small amounts of blood in stools. Every two years, 50-year-olds without symptoms or a family history should take a FOBT.
The test for intestine cancer is not a confirmatory one; rather, it is only a screening one that looks for any source of bleeding from an area of the intestine.
One of the underlying causes of such bleeding may be colorectal cancer. If the test comes back positive, your doctor will provide you with additional information.

Blood in motions can indicate gastrointestinal bleeding, which may be caused by conditions like hemorrhoids or more serious issues such as colorectal cancer.

Diarrhoea, constipation or feeling that the intestine does not empty completely, particularly if this is a change from normal habits. Any persistent or unexplained changes in bowel habits should be promptly evaluated by a healthcare professional.

Blood in vomit and black-colored stool (melena) suggest gastrointestinal bleeding, requiring immediate medical evaluation to determine the underlying cause, which could include stomach ulcers or esophageal varices.

Constant tiredness, weakness, and paleness may signal anemia, often due to conditions like iron deficiency or chronic diseases such as leukemia.

General discomfort in the abdomen can be caused by various conditions, including indigestion, gastritis, or more serious issues like appendicitis or pancreatitis.
Mucus in motions can indicate inflammation of the intestines or infections such as bacterial gastroenteritis, requiring assessment by a healthcare provider to determine appropriate treatment.

Doctors are better able to determine which treatments are most likely to be effective for a given type and stage of cancer thanks to their years of experience treating cancer patients and participating in clinical trials.
Doctors are better able to determine which treatments are most likely to be effective for a given type and stage of cancer thanks to their years of experience treating cancer patients and participating in clinical trials.
You will be advised on the most effective cancer treatment. This will depend on your overall health, the type of cancer you have, where it is and how far it has spread.

This section lists common tests. It is not necessary for all the tests to be performed and your doctor will select the tests that will provide maximum information about the tumor/ disease.
Your doctor will examine you and take a complete medical history before referring you for tests. You may likewise have a blood test and CT Scan to really look at your overall wellbeing.

Test of the rectal area This procedure enables the doctor to examine the last six to eight centimeters of your intestine. Your doctor will feel inside your rectum for anything unusual by inserting a gloved finger into your anus. Although the test may make you feel as though you are about to open your intestines, you won’t lose control.

A CT examine is a sort of x-beam that gives an image of organs and different designs (counting any cancers) in your body. It is used to examine a cancer in greater detail and its relationship to your body’s surrounding organs. It likewise gives data connected with disease spread into the lymph hubs, liver or lungs.

Positron Emission Tomography (PET) Scan This test is combined with a CT scan by injecting a radioactive substance into the body to highlight all of the places where the tumor has or can spread. After an MRI or CT scan, additional information may be gathered through this test. All patients do not require a PET-CT scan. This scan’s necessity will be determined by your physician.

Sigmoidoscopy and colonoscopy In order to view the lining of your intestines, an endoscope, a flexible, lighted tube, will be inserted into your anus. The doctor can use small instruments to insert into the scope and extract some tissue if they notice anything unusual. The tissue can be inspected under a magnifying instrument for a determination.

Endorectal ultrasound scan: If other tests show that you have cancer in your rectum, your doctor may recommend that you have an endorectal ultrasound to learn more about the tumor’s local spread.

A biopsy is a diagnostic procedure performed under a microscope by a pathologist using a small amount of tissue taken from an abnormally found area or lump. If the doctor notices anything unusual during the endoscopy or EUS, they can remove some tissue with small instruments and examine it under a microscope. Cancer has been confirmed by this.

Similar to a CT scan, magnetic resonance imaging (MRI) creates images of your abdomen’s organs using magnetism rather than x-rays. Unlike a CT scan, an MRI does not cause any pain and the magnetism is harmless. In cases of low rectal cancer, an MRI scan may provide more information.

A specific tumor marker test known as CEA (carcinoembryonic antigen) will also be performed in addition to the usual haemoglobin and routine blood tests. Find Here The Best Colon Cancer Treatment In Mumbai The substance (CEA) that is produced in large quantities by intestine cancer cells is the subject of this blood test.

Despite the fact that cancer surgeries are time-consuming and extensive; Surgery has become safer thanks to improved medical care, and surgical instruments are now available. The overall safety of cancer surgical procedures has been significantly improved by improved post-operative monitoring and anesthesia techniques.
Despite the fact that cancer surgeries are time-consuming and extensive; Surgery has become safer thanks to improved medical care, and surgical instruments are now available. The overall safety of cancer surgical procedures has been significantly improved by improved post-operative monitoring and anesthesia techniques.

The position of the tumor in the colon will determine how much of colon is removed. If the left side of the colon is removed, it is called a left hemi colectomy. A temporary colostomy or ileostomy, or diversion of stools, may be performed by the surgeon to allow the area to heal. A few months later, you have another surgery to fix the temporary stoma. This is known as a stoma inversion. You are wearing a colostomy bag over the bowel opening at this time.
Procedures to reduce to chance of this cancer:
Removal of Lymph Nodes Near the Colon All of the lymph nodes near the colon will be removed during the surgery. Lymphadenectomy is the term for this. Lymph nodes are surgically removed because they may contain cancer cells that have separated from the primary cancer.
Sometimes the cancer is very big and can’t be taken out because it is attached to important organs in the abdomen. In the event that this occurs, the surgeon may establish a connection between the intestines prior to and after the blocked site to allow food to pass through the obstruction.
After an anaesthetic, the movement of the bowel slows down and usually takes about 72 hours to get back to normal. After about 48-72 hours you will probably be ready to start taking small sips of water, however your doctors will tell you when it is appropriate for you to start drinking some fluids.
This will be gradually increased after a couple of days until you are able to eat a light diet, usually four or five days after your operation.
You will probably be ready to go home in about two weeks after your operation and once your stitches have been removed. If deemed appropriate your doctor may send you home with stitches and call you later to remove the stitches.
By and large you should be able to climb several flights of stairs after your discharge from the hospital and you will be given diet instructions.
Before you leave hospital you will be given an appointment for a post-operative check-up at the outpatient clinic.
After colon surgery, you can resume your usual diet without restrictions, though initially, certain foods like fruits and vegetables may cause loose stools or affect a colostomy. Individual tolerance varies, so consulting with a hospital dietitian can help manage dietary concerns. Increased bowel movements post-surgery can be addressed with medications prescribed by your doctor, and keeping a food diary can assist in identifying and adjusting to foods that may trigger symptoms.


Dr. Deepak Chhabra is a consultant Surgical Oncologist with an extensive experience in cancer surgeries. He is has specialized in Hepato (Liver) -Biliary (Gallbladder) and Pancreatic Cancer Surgeries.

Take the first step towards your journey to wellness by scheduling an appointment with Dr. Deepak Chhabra, a trusted oncologist dedicated to providing compassionate care and personalized treatment plans.
Discover first hand accounts from patients who have experienced compassionate care and expert treatment at our clinic. Read their reviews to get to know their journey.
